SARS-COV-2 in wastewater: What do we know and challenges ahead?
By Eng. Lakmali Jayaratne & Eng. (Prof) Bandunee AthapattuIntroduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which is the strain of coronavirus that causes coronavirus disease 2019 (COVID-19), the respiratory illness responsible for the COVID-19 pandemic. SARS-CoV-2 previously provisionally named 2019 novel coronavirus or 2019-nCoV. SARS-CoV-2 was discovered in December 2019 in Wuhan (Hubei, China) and the disease quickly spread world-wide due to its high rate of infectivity and the presence of a huge number of asymptomatic carriers, hardly identifiable. In March 2020, the World Health Organization (WHO) declared a pandemic. COVID-19 is affecting many countries and millions of people got infected and died despite various measures taken by those countries.
Coronaviruses is introduced into municipal wastewater through several sources, such as hand washing, sputum and vomit. Additionally, there are reports of viral shedding in urine of individuals infected with SARS-CoV-2. However, the main route that has been reported extensively is via the shedding of the viral RNA in feces of infected individuals.
Due to the urgency of the current COVID-19 pandemic, there are several studies with a wealth of information relevant to SARS-CoV-2 in wastewater were published. One of the reasons for surge interest in the studying of presence of coronaviruses in wastewater is to use this data in wastewater-based epidemiology (WBE). WBE use sewage/untreated wastewater analysis as an early warning system for disease outbreak, since viral RNA can be detected in feces, and subsequently wastewater, weeks before the onset of symptoms in the community.
Further increased interest is due to the possibility of fecal-oral transmission. This is mainly because non enveloped enteric viruses, (e.g., adenoviruses, polioviruses, enteroviruses, noroviruses and rotaviruses) are transmitted primarily through the fecal-oral route. However, according to WHO, there have been no reports of fecal−oral transmission of SARS-CoV-2 to March 29, 2020. Although currently there are no studies available to indicate the transmission of SARS-CoV-2 via sewage or wastewater systems, this hypothesis has not been scientifically eliminated as yet. If confirmed, this may result in far-reaching consequences for public health and for pandemic control strategies.
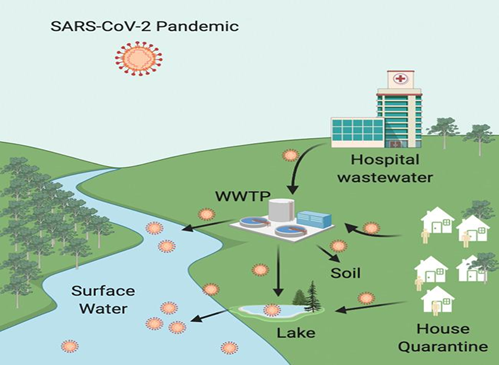
Fig. 1: Possible transport processes of SARS-CoV-2 in the environment.
(Source: https://www.sciencedirect.com/science/article/pii/S0048969720362756#bb0380)
Presence and persistence of SARS-CoV-2 in wastewater
Several studies have shown the presence of the SARS-CoV-2 in feces of infected patients. These results indicate that the viral load in feces is highly variable in the range of 103–107 RNA copies/g feces. SARS-CoV-2 can reach the sewerage via feces beside other human excreta. Recently, the detection of RNA of SARS-CoV-2 in municipal wastewater has been reported from a number of countries including Australia, Spain, Italy, Netherlands and USA. Fig.1 shows the possible transport processes of SARS-CoV-2 in the environment
Some researchers in Australia found that the presence of the virus in the wastewater of the city of Brisbane in the period at the time of the epidemic peak. Although it was detected in two samples, the viral concentration was very low (12 and 1.9 copies/100 ml, respectively). Some researchers in the USA monitored a wastewater treatment plant (WWTP) in Massachusetts showing the presence of SARS-CoV-2 RNA in an order of magnitude, estimated to be 100 viral particles/ml of wastewater. In the Netherlands, researchers studied the wastewater entering eight different WWTPs finding viral fragments of SARS-CoV-2 RNA. The presence of SARS-CoV-2 RNA was detected in Syracuse (New York, USA) in urban sewage during COVID-19 epidemic outbreak. They quantified an average number of 42.7 (±32.9) copies/ml of SARS-CoV-2 RNA with peak of more than 100 copies/ml. During the epidemic peak, in three WWTPs in Paris (France), 106- 107 units/ml of SARS-CoV-2 RNA was measured while in two Spanish regions where COVID-19 had a very low impact, viral RNA in wastewater was collected and quantified as 5.38 ± 0.21 log genomic copies/l. Between February and April, in Milan and Rome (Italy) twelve samples from WWTPs were collected and analyzed. SARS-CoV-2 RNA was evidenced in 50 % of samples.
These studies clearly confirm the presence of SARS-CoV-2 in wastewater although many facts remain uncertain. For instance, it is mandatory to investigate the impact of external conditions, such as temperature, pH and retention time, on the survival of SARS- CoV-2 in wastewater. However, the survival capacity of the virus in wastewater remains largely uncertain and, to date, the results available on the SARS-CoV-2 are limited.
Some researchers recently studied the persistence of RNA of SARS-CoV-2 in untreated wastewater at four different temperatures, i.e., 4, 15, 25, and 37 °C. With an increase in temperature from 4 to 37 °C, the average 90% inactivation was found to decrease from 28 to 8 days, suggesting the persistence of SARS-CoV-2 RNA for several days in untreated wastewater. Additionally, another researcher reported that the virus remained viable for up to 7 days and 14 days in solution when experiments were conducted at room temperature ranging from 20 to 25 °C and 4 °C. However, it was reported that the virus lost its infectivity within 1 to 2 days when the temperature was in the range of 33–37 °C. Solution pH of 5 and 9 resulted in 2.9 and 5.33 log unit loss of infectivity in SARS-CoV-2, respectively, within 6 days. At extreme pH values of 2–3 and 11–12, the virus lost infectivity completely within 1 day.
Though, as SARS-CoV-2 belongs to the coronavirus family, results of some tests conducted assessing the virus survival in hostile environments after the severe acute respiratory syndrome (SARS) epidemic of 2003–2004 is worth mentioning. Some studies had investigated the inactivation time in urban wastewater under different temperature conditions. At low temperatures (4 ◦C) the virus maintained its vitality up to 14 days, while it was inactivated only after 2 days at higher temperatures (20 ◦C). For coronaviruses, survivability at temperatures higher than 20 ◦C was also demonstrated by another study. They observed that human coronavirus 229E inactivates very rapidly in wastewater, with a 99.9%, inactivation in 2–3 days. Survival of the coronavirus in primary wastewater is only slightly longer than secondary wastewater, probably due to the higher level of suspended solids that offer protection from inactivation. They also indicated that coronaviruses might remain stable in wastewater for a longer period than in tap water.
To cause infection, viruses must retain their infectivity until they come in contact with the next host. And test results from RT-qPCR (Reverse Transcription Quantitative Polymerase Chain Reaction), a method recently, widely used to detect and quantify SARS-CoV-2 in wastewater, do not clearly imply that virus is infectious, therefore other approaches must be needed to determine infectivity. And there are no available estimates on the minimal infectious dose (MID) of SARS-CoV-2 in wastewater required for causing infection in humans.
Wastewater treatment and viral removal
There is no evidence to date that the SARS-CoV-2 has been transmitted via sewerage systems with or without wastewater treatment. However, according to WHO, as viral fragments have been found in excreta and because of other potential infectious disease risks from excreta, wastewater should be treated in well-designed and well-managed centralized wastewater treatment works. In conventional WWTPs, disinfection is most commonly carried out by chlorination, UV radiation and Ozone.
Some researchers observed that coronavirus could be inactivated completely after 30 min of disinfection with more than 10 mg/l chlorine (the free residual chlorine was more than 0.4 mg/l) compared to E. coli and bacteriophage viruses. Chlorine dioxide was less effective for the inactivation of coronavirus than chlorine. In another research, it has reported that SARS-
-CoV-2 RNA was in both primary effluent and secondary treated wastewater. When tertiary treatment processes were present in the treatment train, no RNA was detected in the effluent stream (disinfection with NaClO, in some cases coupled with UV). These results were also confirmed by studying the presence of SARS- CoV-2 in several points of a WWTP in Spain. SARS-CoV-2 RNA was detected in the influent to the primary settler (between 7.5 and 15 copies/ml) but not in the secondary treatment effluent, confirming that the effluent is safe for reuse and discharge to water bodies.
Sri Lanka: Current situation and challenges ahead
The number of infections is increasing rapidly in every part of the world including Sri Lanka. It has reported over 35,000 confirmed cases and 176 deaths in Sri Lanka on December 20, 2020. At present, a person who tested positive for coronavirus is transferred to a specific hospital or quarantine centre for treatment.
In Sri Lanka, piped borne sewerage systems cover major urban areas with coverage of 2.1% of the population. Majority of the population relies on on-site sanitation. WHO figures show that sanitation coverage in Sri Lanka is 92%, the best in South Asia. Areas to improve would be including the problem of groundwater contamination resulting from on-site sanitation in congested townships.
Most of the studies published to date on the use of WBE or environmental surveillance for SARS-CoV-2 have been from high-resource settings and suggest that monitoring SARS-CoV-2 in the sewage could offer a cost-effective solution for COVID-19 surveillance. However, lower-resource settings like Sri Lanka, where a greater proportion of the population is not connected to sewers and instead uses septic tanks, needs approaches that can be applied in. Possibilities include testing surface water contaminated by sewage.
Although, at the moment, transmission of SARS-CoV-2 by wastewater has not yet been demonstrated and further studies are required, this aspect is still very important because it could minimize any possible secondary transmission to human and environment. Few reports suggest that there is a potential risk of fecal-oral transmission of COVID-19 in countries with poor wastewater management. This includes risk associated with on-site sanitation. Such systems do not disinfect the effluent. It can contaminate the water bodies with shallow groundwater depth, areas prone to flooding or if open well used for drinking water is located within a distance of 30m from the septic tank if appropriate precautions are not being taken. However, the Environmental Protection Agency (US EPA) expects that a properly managed septic system will treat SARS-COV-2 as the same way it safely manages other viruses often found in wastewater.
In general, WWTPs in Sri Lanka are equipped with necessary technology to remove viruses effectively. In fact, sewage from hospitals and quarantine centres contains SARS-CoV-2, thus requiring efficient disinfection before discharge into water bodies. In addition, actions will be needed where the domestic wastewater contaminated with SARS-CoV-2 is discharged directly into local rivers and streams with limited or no treatment.
In conclusion, the ongoing global pandemic of COVID-19 caused by SARS-CoV-2 has shown increased interest in coronavirus in wastewater. Although the research available in this field is very limited or still in the early stage of development, this article has collected some of the scientific literature currently available in the presence, persistence, and fate of SARS-CoV-2 in wastewater. Studies show that SARS-CoV-2 has been detected in faces and sewage, remains infectious for several days under different environmental conditions and becomes successfully inactivated when disinfected. Present situation in Sri Lanka has also briefly highlighted which further stresses the importance and need for investing in wastewater treatment infrastructure and sanitation in Sri Lanka.
 Eng. Lakmali Jayaratne
Eng. Lakmali Jayaratne
B Sc Civil Engineering, University of Peradeniya
M Sc Environmental Engineering and Management, University of Moratuwa
Associate Member of IESL
 Eng. (Prof) Bandunee Athapattu
Eng. (Prof) Bandunee Athapattu
B.Sc. (Civil Eng), M.Eng (Env Eng), Ph.D. (Env Eng)
Professor, Department of Civil Engineering,
Open University of Sri Lanka
Chartered Engineer, Member of IESL
Member of IWA, Section C - SLAAS





